HL7 is an international standard or protocol that ensures the transfer of patient information from one system to another in a correct and logical manner. The hospital systems are required to communicate with each other or allow the sharing of information whenever it is needed. Every hospital has at least a basic system for capturing patient information, and whenever new information is added, it gets updated.
The challenge is to have a common method even if the patient visits multiple hospitals. The care providers need to have a complete history of the patient’s history, medical conditions, etc. before starting treatment. Founded in 1987 by Donald W. Simborg, the CEO of Simborg Systems, HL7 focuses on the application layer protocols pertaining to the healthcare domain. There are several versions of HL7, and the most commonly used is the HL7 version 2.x family. HL7FHIR is the newest generation standards framework. It combines all the features of HL7 Version 2, Version 3 and CDA® product lines, and offers significant improvements over existing standards. FHIR, short for Fast Healthcare Interoperability Resource and pronounced as FIRE, is really becoming the next big thing in the healthcare industry right now because of its capabilities.
Cabot has been pioneers in HL7 FHIR Interface Software Development Services and it gives us immense joy in explaining a bit deeper into why HL7 and FHIR are so important in uninterrupted health care.

Image Credit: HL7.org
This is how the processing of healthcare data is done:
Once the patient meets with a doctor, the doctor refers to the HIS (or the Hospital Information System) to get background information on the patient, and the doctor's suggestions (blood tests, X-rays, other tests, etc.) will also be entered into the HIS. This information would then be accessed by other medical staff and entered into their computer systems. The patient might even be referred to a different hospital to commence treatment.
Now, this is where HL7 comes into the picture. HL7 or Health Level 7 is a set of standards that are used for moving or disseminating a patient’s clinical and administrative data between one or more hospital information systems. HL7 can also be called a ‘language’ that’s communicated to different medical systems. The language will be all about the patient, his/her complete medical information, demographics and other relevant information. All this information would then be packaged and stored, so every authorized person or organization can access it. Everything is done to provide accurate and efficient patient-centered care.
The current version of FHIR is touted to be the most expressive one when compared to the HL7 standards like Version2, 3 and CDA. HIT vendors like Epic, Allscripts and Cerner are already adopting this standard on a bigger scale.
The pace at which FHIR enabled interoperability is moving is incredibly swift, especially since interoperability is also making its strong presence known.
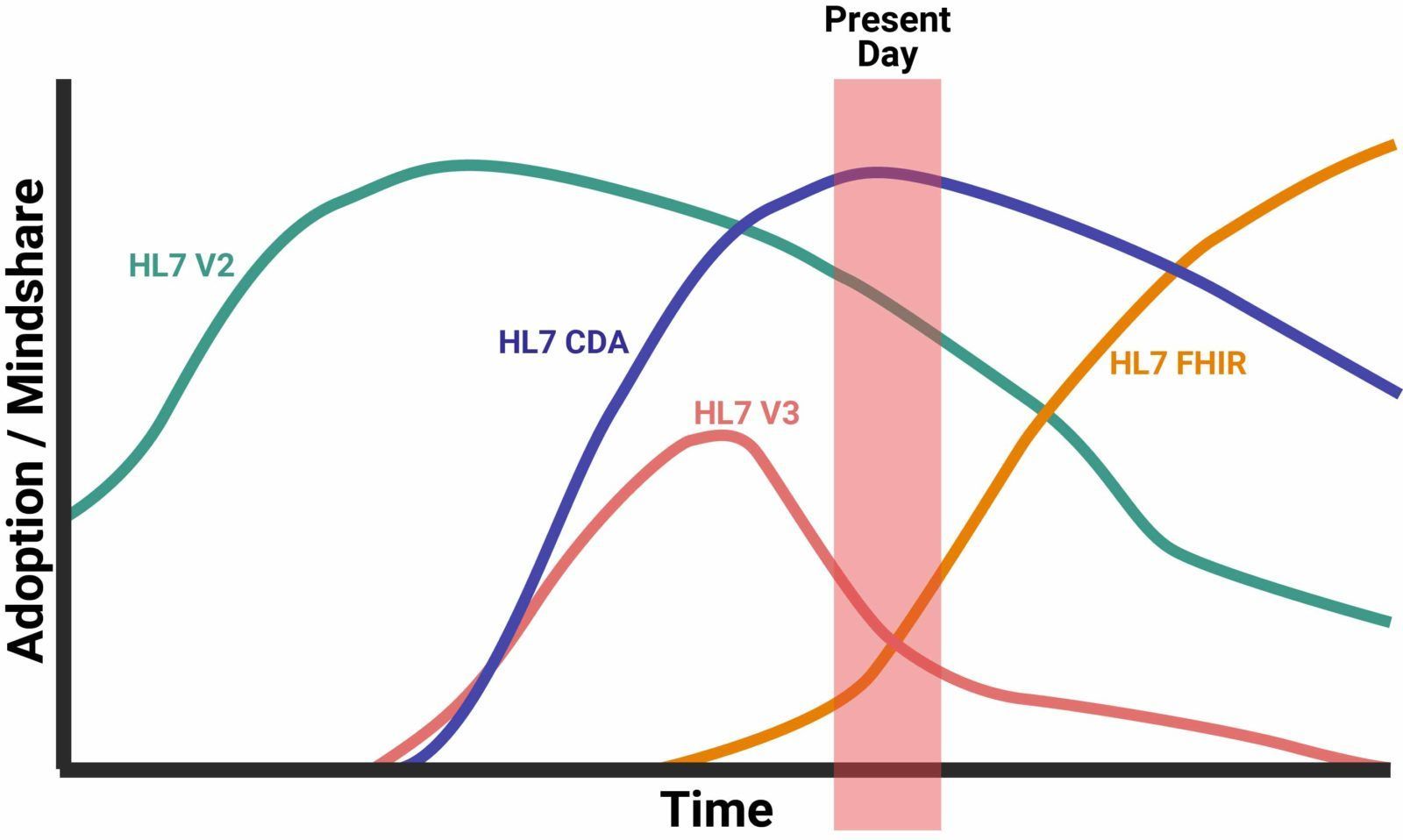
Image Credit: InterSystems
There are many reasons for this. Let’s look at three:
(a) Apple, a major player in mobile devices, made its announcement by including FHIR in iOS devices. It doesn’t come as an app but is included in the operating system itself. And then you have the Apple Health Records option. Initially, Apple started with 12 university health systems, then it grew to 500 and the number is still growing.
(b) Another change was the launch of the Da Vinci project. This payer-focused program was started in January 2018 with the help of some very major players participating in it, like United Healthcare, BlueCross BlueShield Association, Anthem and so on. Initially, the insurance companies were not keen on joining the path, but once they understood the importance of claims data and how they can really shape healthcare, they agreed to be a part of it.
(c) The most noted forward movement in FHIR happened when the most powerful giants in the industry took a vow to accelerate interoperability in healthcare by making use of the latest cloud-based technologies and Artificial Intelligence to provide excellent care to patients. Big shots like Amazon, Google, Microsoft, Salesforce, IBM, and Oracle signed this joint pledge in August.
HL7 can make a significant change in the way patient care is delivered. This is a reliable standard that combines all the best features from HL7 v2, HL7 v3, and CDA, and also all the improvements made after observing the shortcomings in the previous standards. Apart from being the best of all worlds, there are other reasons why implementing FHIR is the next big thing in healthcare:
It is developer-friendly - The specification helps share data in a modern and developer-friendly way. This is because it uses all the familiar tools that developers are already familiar with, for example, HTTPS, REST, XML, JSON, ATOM, and OAuth. The developers don’t have to study any particular technology to work with FHIR.
FHIR is open source and free to use - FHIR, with its open APIs helps in continuous real-time data exchange, makes it easy for developers to access healthcare data from healthcare applications.
Specifications for HL7 is free - All that you need to develop and implement systems that can communicate through FHIR is free. No login is required, nor is the developer under any restrictions.
It is fast and easy to implement - A strong focus of this standard is that it is fast and easy to implement. If there are multiple developers working on a project, and with the compatible interaction engine, they can have a simple interface working in just one day.
Cost savings because of the use of well-known web technologies - Anyone working in website building or web technologies can develop applications with FHIR. So, if you are building your team to accommodate HL7 FHIR, the pool of candidates would be much bigger and deeper.
It is greatly suitable for mobile apps - There has been a huge rise in mobile health applications, especially HTTP REST and JSON. FHIR supports all the technologies that mobile devices also use, increasing the capacity of interoperability several times over.
More granular way exchanging data - The workflow module of FHIR focuses on the co-ordination of sharing data across different systems, and hence much more granular than the traditional HL7.
It keeps the 80/20 rule - A good thing about FHIR is that the focus will be on 80% of the common use cases rather than the 20%. So the real patient would benefit from it, rather than just the exceptional cases.
Perfect for Connectathons - Connectathon is the healthcare industry’s most vigorous and supervised testing event for interoperability. The testing is done between vendors for a period and it's live to enable a detailed implementation and testing process. Thousands of vendors participate in the testing events held in Asia, North America and Europe.
Though FHIR can ease interoperability across systems in a dynamic manner, the standard does have some points that make it both strong and weak. Of course, it is much more capable and expressive than the previous HL7 standards (Version2, 3 and CDA) and the implementers can attain much more accurate queries, but there are still some drawbacks that need to be cleared.
1. A simple query will give instant results
One of the major differences FHIR has with HL7 is that just a simple query will give you accurate results. With HL7 CDA, you need to go retrieve and parse through the entire document in detail, even if you were looking for simple information such as a patient’s allergies. In FHIR, all you need to do is type in the simple query and the relevant information would come in. As the level of complexity increases, the implementers can apply those in the query. For example, allergy to a particular food item might need a specific request, rather than just allergies.
2. Create apps that can make use of the functionalities of underlying systems
By creating innovative apps, it is possible to increase the functionalities of the underlying systems, meaning Electronic Health Records. For example, a team of heart specialists can pull out the best treatment regime for a heart problem by pulling out the necessary and relevant information from the physician's records and create apps with similar information about various conditions.
3. FHIR benefits the most reluctant category - the payers
The most reluctant category in FHIR interoperability are the payers, but they have also changed their views lately. Payers collate their customers’ clinical records and they have access to all information collected from everywhere - EMR, HIE, third-party vendors and so on. They can provide the missing clinical piece and make use of FHIR for eligibility verification as well.
4. Cost-saving for the healthcare IT teams
Developers engaging in HL7 FHIR interface software development can make use of all the popular web technologies in the industry to make apps. This is a huge cost-saving factor since you can hire developers easily, and there is a large pool of skilled experts to choose from.
1. Constant vigilance and testing is important
Interoperability is perhaps at its nascent stage still because you still have to go through the slow and painstaking task of seamless interoperability between different systems. FHIR is an international standard, so it may not always be compatible with all. And you need to ensure that the validation and testing tools work towards server compliance as per FHIR specifications.
2. Data matching issues are quite rampant
Another challenge faced with FHIR is that the data may not always be the same. For example, take lab results for instance. If there is no common matching technology, then having a vendor-EHR specific terminology is practically not possible. This causes data matching issues. If there is common terminology for all such medical requirements, much of the challenges can be solved.
3. Current iterations of the FHIR standard are not backward-compatible
Unfortunately, some of the features of FHIR also contribute to its disadvantages. Right from the release of FHIR 4, certain portions must be normative (any changes made to its portions will make it backward compatible). FHIR deals on extension mechanisms so implementers have several different ways of performing the same action, rather than handling use cases. It backfires when different implementers extend FHIR differently.
4. Patient matching could be a problem
Simple changes in patient information can be a problem when you want to access data from across different systems. A slight mistake in the social security number, a dash or spelling change in the name could cause problems. If there is a matching algorithm and global identifier that can connect when the same patient logs in from a different hospital or institution, then the global identifier can prove that it is the same patient.
FHIR is still young as it was released only in 2017, so the APIs are still evolving. However, it has moved in from the fringes to the mainstage. Once the versions change and new requirements come in, the APIs will have to be changed accordingly. Nevertheless, in a few years' time, you can expect stable FHIR implementation standards.
Is your healthcare organization already using FHIR as a tool to improve the interoperability of health data with other systems? If not, you need to adopt it as soon as possible. Now, HL7 has developed into an international organization with over 50 countries as members, and these are some of the biggest players in the industry, including vendors and healthcare providers. It is true that there are improvements that need to be made, and some providers and payers still have to join the club. The funding for this also has to be improved in order to have faster progress of FHIR HL7.
Using a multiyear balloting system, new standards are being developed in HL7, where members vote and analyze for negative comments. All of them study the draft comments, and they would be tested through trials until the standards become formal and adaptable. All the members would then adopt these formal standards.
Maintaining interoperability can be successful only when there is constant vigilance and continuous testing. FHIR is right at the center of it, and can revolutionalize HIT in the long run. As of today, we still have to perfect the slow and tedious work of ensuring there is interoperability between multiple systems. Imagine going to the grocery store. Just standing there looking at the ingredients will not put dinner for your family. You still have to buy all of the ingredients and in the right quantity to prepare a tasty dinner. That’s the state of HL7 FHIR adoption as well.
Want to jump onto the HL7 FHIR bandwagon? Let us assist you!


YOU WILL BE HEARING FROM US SOON!
We look forward to hearing from you!

YOU WILL BE HEARING FROM US SOON!